eMedicine Specialties > Radiology > Brain/Spine
Multiple Sclerosis, Spine
Djamil Fertikh, MD, Attending Physician, Division of Radiology, Association of Alexandria Radiologists
Michael L Brooks, MD, JD, FCLM, Clinical Associate Professor of Radiology, Philadelphia College of Osteopathic Medicine; Director of Neuroradiology, Mercy Diagnostic Imaging, Department of Radiology, Mercy Fitzgerald Hospital
Updated: May 24, 2008
Introduction
Background
Multiple sclerosis (MS) is considered the most common demyelinating process involving the central nervous system (CNS).1 In 1988, MS was first described in the upper cervical spine using magnetic resonance imaging (MRI). Spinal MS is often associated with concomitant brain lesions; however, as many as 20% of patients with spinal lesions do not have intracranial plaques. No strong correlation has been established between the extent of the plaques and the degree of clinical disability.
For excellent patient education resources, visit eMedicine's Muscle Disorders Center. Also, see eMedicine's patient education article Multiple Sclerosis.
Related eMedicine articles:
Brain, Multiple Sclerosis
Multiple Sclerosis [Emergency Medicine]
Multiple Sclerosis [Neurology]
Multiple Sclerosis [Ophthalmology]
Multiple Sclerosis [Physical Medicine and Rehabilitation]
Related Medscape topic:
Resource Center Multiple Sclerosis
Pathophysiology
The exact cause of MS remains unclear; however, hypotheses include viral and autoimmune etiologies.
In the acute stage, perivenular inflammation with hypercellularity (macrophages and/or lymphocytes) is encountered in typically well-demarcated areas of demyelination.
In the chronic stages of the disease, fibrillary gliosis occurs with a breakdown of myelin. The axonal structure is conserved, with a reduction or absence of oligodendroglia. Occasionally, lesions resolve incompletely, but most progress to demyelination.
Frequency
United States
There are an estimated 250,000-350,000 patients in the United States with MS.
International
MS occurs worldwide.2 Its prevalence varies depending on the geographic location, rising as the northerly or southerly distance from the equator increases. Depending on the country or the specific population, the prevalence of MS ranges from 2 cases per 100,000 population to 150 cases per 100,000 population.
Related Medscape topic:
CME The Impact and Burden of Multiple Sclerosis
Mortality/Morbidity
- The morbidity and mortality rates related to MS are high worldwide.
- At 15 years after the onset of the disease, an estimated 50% of patients need help with ambulation.
Related Medscape topics:
CME Evaluating New Data for the Treatment of MS
CME/CE Specialty Pharmacy & Treatment Optimization: Applications for the Multiple Sclerosis Population
Race
Epidemiologic series have shown that western Europeans living in temperate zones have a higher risk for MS than do other groups.
Sex
The male-to-female ratio is 2:3.
Age
MS frequently occurs in persons aged 10-50 years. However, MS has also been described in the pediatric population and in individuals older than 50 years.
Anatomy
Spinal MS has a predilection for the cervical spinal cord (67% of cases), with preferential, eccentric involvement of the dorsal and lateral areas of the spinal cord abutting the subarachnoid space around the cord. The gray matter may be involved. Approximately 55-75% of patients with MS have spinal lesions at some point during the course of the disease.
Presentation
The clinical signs vary depending on the spinal cord segment affected and the degree of involvement. MS is characterized by a typical relapsing-remitting clinical course. Spastic paraparesis/paraplegia with neurogenic bowel and bladder, as well as with sexual dysfunction, can be encountered. Dysesthetic pain syndromes may result from spinal or cranial nerve root involvement.
Heredity is suggested to be involved in the etiology of the disease because affected relatives occasionally are identified.
A concomitant presence of optic neuritis (unilateral, bilateral, or chiasm) constitutes Devic neuromyelitis optica. The brain is usually normal, but the condition is associated with a poor prognosis.
MS can be seen with Leber hereditary optic neuropathy, which is called Harding's syndrome.3
Preferred Examination
Although nonspecific, MRI is presently considered to be the most sensitive diagnostic imaging modality for revealing demyelinating plaques. MRI shows abnormalities in 95% of patients with clinically definitive MS.4, 5
Limitations of Techniques
MRI is sensitive to areas of demyelination, which appear as high signal areas on long TR sequences. Lesions of other etiologies (eg, viral myelitis, acute disseminated encephalomyelitis [ADEM]) may resemble MS plaques and must be considered along with the clinical history and the patient's presenting signs and symptoms.
Differential Diagnoses
Sarcoidosis
Systemic Lupus Erythematosus
Other Problems to Be Considered
Spinal cord tumors (primary or metastasis)
Infection (particularly viral, eg, cytomegalovirus, herpes, human immunodeficiency virus [HIV])
Acute transverse myelitis (history of recent viral infection or vaccination)
Acute spinal cord infarction (acute presentation)
Radiation myelitis (generally doses >4000 cGy; 1- to 3-y latency period; chemotherapy may be synergistic)
Computed Tomography
Findings
With the advancement of MRI, evaluation of the spinal cord using axial computed tomography (CT) scanning was abandoned because of its poor sensitivity. Large, masslike lesions can occasionally mimic a neoplasm, and characterizing them can be difficult.
Degree of Confidence
As a result of CT scanning's poor sensitivity, the detection, evaluation, and characterization of MS lesions and enhancement patterns are limited with this modality.
False Positives/Negatives
Primary and secondary neoplasms of the spinal cord (astrocytomas, ependymomas), infection, transverse myelitis, acute infarction, sarcoidosis, and systemic lupus erythematosus may mimic demyelinating MS plaques.
Magnetic Resonance Imaging
Findings
MRI far exceeds CT scanning in the ability to demonstrate intramedullary pathology; MRI is currently used for the first-line investigation.6
Depending on their age, MS plaques appear on unenhanced, T1-weighted images as areas of slightly low to low signal intensity. Plaques may appear as nodules, rings, or arcs and generally are less than 2 vertebral bodies in length.7 Plaques usually demonstrate prompt enhancement after the administration of a gadolinium-based contrast agent, which most often indicates active disease.8 The enhancement may last 2-8 weeks. Steroids typically do not suppress the enhancement of the active plaques. Classic chronic lesions do not demonstrate contrast enhancement.
Most MS plaques appear hyperintense on T2-weighted images. The spinal cord may or may not be focally enlarged. Enlargement of the cord is usually seen with active disease. Larger active lesions may have extensive edema with associated cord expansion. Chronic lesions often demonstrate focal cord atrophy. Spinal lesions usually coexist with more severe concomitant brain plaques. As many as 20% of spinal MS lesions are isolated. Spinal cord narrowing due to atrophic changes is present in 10% of patients with spinal cord involvement.
Tumefacient MS may mimic a neoplasm; a demyelinating process should always be considered if a masslike lesion is encountered. As is the case in the brain, a ring or arc of enhancement can often be found, as opposed to a more nodular or masslike enhancement. Follow-up studies are helpful.
Although not widely implemented, newer methods may be more specific in evaluating MS plaques.9 These methods include magnetization transfer and diffusion, as well as proton magnetic resonance spectroscopy (MRS).10, 11
Typically, fast-FLAIR (fluid-attenuated inversion recovery) sequences have been shown to have a lower sensitivity than do fast spin-echo sequences (FSE) for depicting spinal cord MS lesions.12, 13, 14
Studies have suggested that more cervical cord MS lesions can be revealed with magnetization transfer–prepared gradient-echo and fast-STIR (short TI inversion recovery) sequences than with FSE sequences, with fast-STIR demonstrating the greatest sensitivity.13, 15, 16, 17, 18
Gadolinium-based contrast agents (gadopentetate dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance], gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol [ProHance]) have recently been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more information, see the eMedicine topic Nephrogenic Fibrosing Dermopathy. The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or magnetic resonance angiography (MRA) scans.
As of late December 2006, the Food and Drug Administration (FDA) had received reports of 90 such cases. Worldwide, over 200 cases have been reported, according to the FDA. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness. For more information, see the FDA Public Health Advisory or Medscape.
Degree of Confidence
Although MRI is not specific, it is considered the most sensitive imaging modality for diagnosing spinal cord MS, for evaluating its extent, and for following up the response to treatment. MRI is more sensitive for identifying active plaques than is double-dose CT scanning or clinical examination.
False Positives/Negatives
The main differentials include, but are not limited to, the following:
- Primary or metastatic spinal cord neoplasms (eg, astrocytomas, ependymomas) - The presence of cysts and hemorrhage support the diagnosis of neoplasm.
- ADEM - This may show enhancement. The concomitant presence of brain lesions is the rule. It runs a monophasic course; therefore, it does not have the relapsing course of MS. A history of viral infection within the previous 3-4 weeks should alert the radiologist. ADEM is typically monophasic.
- Sarcoidosis - This involves the CNS in approximately 5% of cases. Concomitant pial involvement is frequently encountered. Enhancement is usually the rule.
- Transverse myelitis - This term is usually used for idiopathic inflammatory myelopathy. Cord swelling and enhancement may be present, often involving a longer segment than MS. MRI of the brain may be helpful for showing additional lesions in case of MS or ADEM. This condition usually responds to steroid therapy; therefore, a treatment trial is often considered before proceeding with biopsy. This process is typically monophasic.
- Infarct - This is more common at the thoracic level. Usually, only a single lesion is present. Contrast may be present, although this is not the dominant feature. Signal alteration usually and initially involves the anterior gray matter (anterior spinal artery distribution). The patient's clinical presentation will be acute. Particularly consider this entity if the patient is older and/or has a history of aortic/vascular surgery.
- Vasculitis - Processes such as systemic lupus erythematosus can result in spinal lesions that mimic MS. Often, multiple lesions are present. However, the clinical history is often known and helps to establish the correct diagnosis.
- Radiation myelitis - Generally, doses higher than 4000 cGy are required to cause this condition. The latency period is 1-3 years. Chemotherapy may be synergistic. Images may show some peripheral enhancement.
- Arteriovenous fistula - Usually, this occurs at the thoracolumbar level, and patients are usually older than 50 years, with a long history of back pain. The cord signal abnormality can involve a very long segment. Look for a serpiginous flow void along the cord surface.
Intervention
Medicolegal Pitfalls
- Abnormal spinal cord lesions do not always represent neoplasms. A repeat examination should always be considered in suspicious cases.
- Careful review of the patient's medical history and an evaluation of the brain with MRI can prove helpful in the diagnosis, especially in young females.
Multimedia
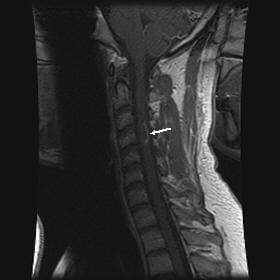
Media file 1: Sagittal, T2-weighted magnetic resonance image of the cervical spinal cord in a 27-year-old woman showing a fusiform area of increased signal intensity representing a multiple sclerosis plaque. Same patient as in Image 2.
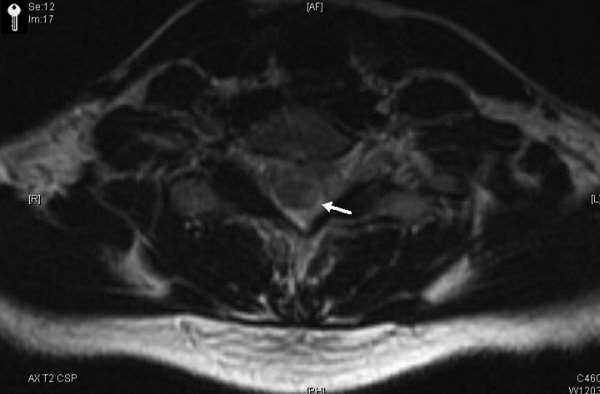
Media file 2: Corresponding axial, T2-weighted magnetic resonance image in a 27-year-old woman showing a multiple sclerosis plaque located in the left dorsolateral region of the left hemicord. Same patient as in Image 1.
Media file 3: Sagittal, T2-weighted image showing areas of signal hyperintensity in the cervical spinal cord and pons. Same patient as in Images 4-5.
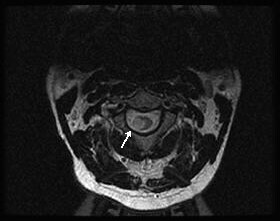
Media file 4: Corresponding axial, T2-weighted image showing a large area of signal hyperintensity in the right lateral aspect of the cord. Same patient as in Images 3 and 5.
Media file 5: Sagittal, T1-weighted image following gadolinium contrast showing arciform enhancement along the edge of the plaque, typical of demyelination. Same patient as in Images 3-4.
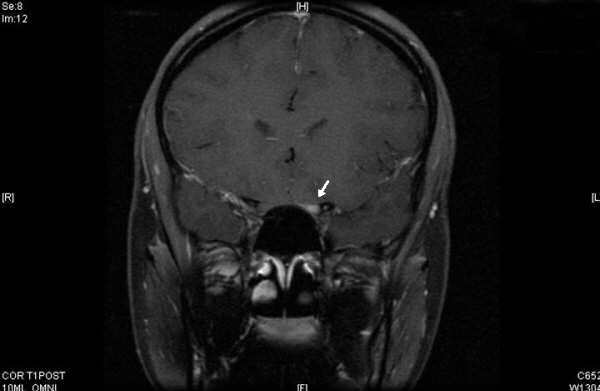
Media file 6: Gadolinium-enhanced, T1-weighted image showing enhancement of the left optic nerve (arrow). Same patient as in Image 7.
Media file 7: Corresponding axial images of the spinal cord showing enhancing plaque (arrow). The combination of optic neuritis and spinal cord lesion constitutes Devic neuromyelitis optica. Same patient as in Image 6.
Media file 8: Sagittal, T2-weighted image showing a focal area of spinal cord atrophy in a patient with long-standing multiple sclerosis.
References
Noseworthy JH, Lucchinetti C, Rodriguez M, et al. Multiple sclerosis. N Engl J Med. Sep 28 2000;343(13):938-52. [Medline].
Rosati G. The prevalence of multiple sclerosis in the world: an update. Neurol. Sci. 2001;22 (2):117–39. [Medline].
Parry-Jones AR, Mitchell JD, Gunarwardena WJ, et al. Leber's hereditary optic neuropathy associated with multiple sclerosis: Harding's syndrome. Pract Neurol. Apr 2008;8(2):118-21. [Medline].
Grossman RI, Yousem DM. Neuroradiology: The Requisites. St Louis, Mo: Mosby-Year Book; 1994.
Rovira-Canellas A, Alonso-Farre J, Rio-Izquierdo J. [Magnetic resonance in the clinical and therapeutic follow-up of multiple sclerosis]. Rev Neurol. May 16-31 2000;30(10):980-5. [Medline].
Agosta F, Absinta M, Sormani MP, et al. In vivo assessment of cervical cord damage in MS patients: a longitudinal diffusion tensor MRI study. Brain. Aug 2007;130:2211-9. [Medline].
LM Tartaglino, DP Friedman, AE Flanders, et al. Multiple sclerosis in the spinal cord: MR appearance and correlation with clinical parameters. Radiology. 1995;Vol 195:725-32. [Medline]. [Full Text].
Filippi M. Enhanced magnetic resonance imaging in multiple sclerosis. Mult Scler. Oct 2000;6(5):320-6. [Medline].
Grossman RI, Barkhof F, Filippi M. Assessment of spinal cord damage in MS using MRI. J Neurol Sci. Jan 15 2000;172 Suppl 1:S36-9. [Medline].
Henning A, Schär M, Kollias SS, et al. Quantitative magnetic resonance spectroscopy in the entire human cervical spinal cord and beyond at 3T. Magn Reson Med. Apr 17 2008;[Medline].
Marliani AF, Clementi V, Albini-Riccioli L, et al. Quantitative proton magnetic resonance spectroscopy of the human cervical spinal cord at 3 Tesla. Magn Reson Med. Jan 2007;57(1):160-3. [Medline].
Filippi M, Yousry TA, Alkadhi H, et al. Spinal cord MRI in multiple sclerosis with multicoil arrays: a comparison between fast spin echo and fast FLAIR. J Neurol Neurosurg Psychiatry. Dec 1996;61(6):632-5. [Medline]. [Full Text].
Hittmair K, Mallek R, Prayer D, et al. Spinal cord lesions in patients with multiple sclerosis: comparison of MR pulse sequences. AJNR Am J Neuroradiol. Sep 1996;17(8):1555-65. [Medline]. [Full Text].
Stevenson VL, Gawne-Cain ML, Barker GJ, et al. Imaging of the spinal cord and brain in multiple sclerosis: a comparative study between fast FLAIR and fast spin echo. J Neurol. Feb 1997;244(2):119-24. [Medline].
Filippi M, Bozzali M, Horsfield MA, et al. A conventional and magnetization transfer MRI study of the cervical cord in patients with MS. Neurology. Jan 11 2000;54(1):207-13. [Medline].
Finelli DA, Hurst GC, Karaman BA, et al. Use of magnetization transfer for improved contrast on gradient-echo MR images of the cervical spine. Radiology. Oct 1994;193(1):165-71. [Medline]. [Full Text].
Rocca MA, Mastronardo G, Horsfield MA, et al. Comparison of three MR sequences for the detection of cervical cord lesions in patients with multiple sclerosis. AJNR Am J Neuroradiol. Oct 1999;20(9):1710-6. [Medline]. [Full Text].
Poonawalla AH, Hou P, Nelson FA, et al. Cervical spinal cord lesions in multiple sclerosis: T1-weighted inversion-recovery MR imaging with phase-sensitive reconstruction. Radiology. Jan 2008;246(1):258-64. [Medline]. [Full Text].
Keywords
MS, demyelinating process, brain lesions, spine lesions, perivenular inflammation, plaques, fibrillary gliosis, oligodendroglia, spinal MS, spinal multiple sclerosis, Devic neuromyelitis optica, optic neuritis
Contributor Information and Disclosures
Author
Djamil Fertikh, MD, Attending Physician, Division of Radiology, Association of Alexandria Radiologists
Djamil Fertikh, MD is a member of the following medical societies: American College of Radiology, American Medical Association, and Radiological Society of North America
Disclosure: Nothing to disclose
Coauthor
Michael L Brooks, MD, JD, FCLM, Clinical Associate Professor of Radiology, Philadelphia College of Osteopathic Medicine; Director of Neuroradiology, Mercy Diagnostic Imaging, Department of Radiology, Mercy Fitzgerald Hospital
Michael L Brooks, MD, JD, FCLM is a member of the following medical societies: American College of Legal Medicine, American College of Radiology, American Society of Neuroradiology, American Society of Pediatric Neuroradiology, and American Society of Spine Radiology
Disclosure: Nothing to disclose
Medical Editor
Mahesh R Patel, MD, Chief of MRI, Department of Radiology, Santa Clara Valley Medical Center
Mahesh R Patel, MD is a member of the following medical societies: Radiological Society of North America
Disclosure: Nothing to disclose
Pharmacy Editor
Bernard D Coombs, MB, ChB, PhD, Consulting Staff, Department of Specialist Rehabilitation Services, Hutt Valley District Health Board, New Zealand
Disclosure: Nothing to disclose
Managing Editor
Val Runge, MD, Robert and Alma Moreton Centennial Chair in Radiology, Professor, Editor-in-Chief of Investigative Radiology, Department of Radiology, Scott and White Clinic and Hospital
Val Runge, MD is a member of the following medical societies: Society for Health and Human Values
Disclosure: Nothing to disclose
CME Editor
Robert M Krasny, MD, Consulting Staff, Department of Radiology, The Angeles Clinic and Research Institute
Robert M Krasny, MD is a member of the following medical societies: American Roentgen Ray Society and Radiological Society of North America
Disclosure: Nothing to disclose
Chief Editor
James G Smirniotopoulos, MD, Professor of Radiology, Neurology, and Biomedical Informatics, Chairman, Department of Radiology and Radiological Sciences, Uniformed Services University of the Health Sciences
James G Smirniotopoulos, MD is a member of the following medical societies: American College of Radiology, American Roentgen Ray Society, American Society of Head and Neck Radiology, American Society of Neuroradiology, American Society of Pediatric Neuroradiology, Association of University Radiologists, and Radiological Society of North America
Disclosure: Nothing to disclose
© 1994-2009 by Medscape.
All Rights Reserved
(http://www.medscape.com/public/copyright)







3 comments:
Intervention AE is a television series that illustrates the lives of individuals who suffer from some form of addiction or compulsive behavior. The show highlights the various intervention strategies used by the family members and friends of these individuals, and aims to provide hope to others out there who are suffering from similar ailments.
Great article. This is one of the good ways that radiologists can learn new stuff or refresh their memories - another way of doing this is by taking up radiology continuing education programs.
Hello everyone, i'm Linda Harry from United State i was diagnosed with Parkinson Disease for over 6 years which made me loose my job and my relationship with my Fiance after he discovered that i was having Parkinson, he departed from me, and i tried all my best to make him stays, but he neglected me until a friend of mine from UK told me Great healer, who will restore my life back with his powerful healing herbal medicine. then he sent me his email address to contact him- drimolaherbalmademedicine@gmail.com. and i quickly contacted him, and he said my condition can be solved, that he will treat the disease immediately only if i can accept trust on him and accept his terms and condition, i Agreed because i was so much in need of help by all means, so i did all he instructed me to do. And surprisingly after two weeks, He sent me a text, that i should hurry up to the hospital for a checkup, which i truly did, i confirm from my doctor that i am now ( PARKINSON NEGATIVE) my eyes filled with tears and joy, crying heavily because truly the disease deprived me of many things from my life, This is a Miracle, dr imoloa also uses his powerful herbal medicine to cure the following diseases: lupus disease, mouth ulcer, mouth cancer, body pain, fever, hepatitis A.B.C., syphilis, diarrhea, HIV/AIDS, Huntington's Disease, back acne, Chronic renal failure, addison disease, Chronic Pain, Crohn's Disease, Cystic Fibrosis, Fibromyalgia, Inflammatory Bowel Disease, fungal nail disease, Lyme Disease, Celia disease, Lymphoma, Major Depression, Malignant Melanoma, Mania, Melorheostosis, Meniere's Disease, Mucopolysaccharidosis , Multiple Sclerosis, Muscular Dystrophy, Rheumatoid Arthritis, Alzheimer's Disease, parkison disease, vaginal cancer, epilepsy, Anxiety Disorders, Autoimmune Disease, Back Pain, Back Sprain, Bipolar Disorder, Brain Tumour, Malignant, Bruxism, Bulimia, Cervical Disk Disease, cardiovascular disease, Neoplasms, chronic respiratory disease, mental and behavioural disorder, Cystic Fibrosis, Hypertension, Diabetes, asthma, Inflammatory autoimmune-mediated arthritis. chronic kidney disease, inflammatory joint disease, impotence, feta alcohol spectrum, Dysthymic Disorder, Eczema, tuberculosis, Chronic Fatigue Syndrome, constipation, inflammatory bowel disease, bone cancer, lung cancer. contact him on email- drimolaherbalmademedicine@gmail.com. and also on whatssap- +2347081986098
Post a Comment