Synopsis
Background: Widespread use of ultrasound to assess thyroid disease has led to an increased number of clinically unapparent, nonpalpable nodules being identified. Although many of these nodules are benign, malignancy cannot be excluded without further testing by fine-needle aspiration cytology (FNAC).
Objective: To evaluate whether ultrasound criteria can be used to identify malignant nodules and, therefore, limit the number of patients undergoing unnecessary FNAC.
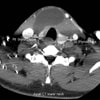
Design and Intervention: This study evaluated patients referred to the thyroid unit at the University of Brescia, Italy, a geographic region with endemic goiter. Inclusion criteria included normal thyroid function, ultrasound identification of a solid, nonpalpable nodule and no previous diagnosis of thyroid malignancy. Ultrasound was performed using a real-time scanner and the following parameters were assessed: echographic dimension (anteroposterior and transverse diameter), echogenicity, calcification, lesion margins (well-defined or blurred), and vascularity pattern. FNAC was performed using 25-gauge needles and lesions were classified as benign, suspicious, or malignant. Patients with suspicious or malignant cytology underwent surgery; those with benign nodules received follow-up ultrasound after 6 months.
Outcome Measures: The main outcome measures were ultrasound and FNAC.
Results: A total of 701 nodules were examined; 327 were solitary and 374 were embedded in a multinodular goiter. FNAC identified 108 (15.4%) of the nodules as suspicious or malignant. Histology after surgery confirmed that 67 of these were carcinomas (50 papillary, 15 follicular, and 2 medullary) and 41 were adenomas. Extracapsular growth was present in 8 carcinomas and was predicted by ultrasound in one case. Additionally, lymph node metastases were detected in 16 carcinomas, 3 of which were predicted by ultrasound. When ultrasound parameters were related to histology, malignant nodules were more likely than benign nodules to present with an anteroposterior to transverse diameter ratio (A/T)≥1 (83.6% versus 18.5%; P <0.001). A similar trend was observed for the other sonographic criteria, although no single parameter identified a subset of patients requiring FNAC. Carcinomas presented with a solid, hypoechoic appearance in 79.1% of cases, blurred margins in 47.8%, microcalcification in 73.1%, and intranodular vascularity in 56.7%. All variables were found to be independent risk factors for malignancy (odds ratio 2.6�22.4). Combining an A/T≥1 with at least one of these variables gave the greatest sensitivity (83.6%) and specificity (91.9%), limiting the need for FNAC to only 15.9% of the nodules.
Conclusion: Combining an A/T≥1 with at least one other sonographic criterion to predict which nonpalpable nodules are malignant could be an effective tool to select patients for FNAC, reducing the number of unnecessary procedures currently performed.
Commentary
Before the introduction of high-frequency ultrasound for evaluating the thyroid gland, nonpalpable nodules were detected in about 6% of the adult population; however, ultrasound now detects such nodules in more than half of the general population aged over 50 years. As only 4-7% of nodules are malignant, the challenge for clinicians is to devise a rational strategy to differentiate lesions that require surgical excision from those that can be followed medically.[1,2] Before diagnostic ultrasound, the decision to perform FNAC was based predominantly upon nodule size. With ultrasound imaging, however, the number of nodules that meet any specific size cutoff has increased. In an attempt to provide a framework for triaging nodules for FNAC according to the highest risk of malignancy, sonographic features of nodules associated with thyroid cancer have been identified.[3]
The results from Cappelli et al. are consistent with previously published sensitivity and specificity estimates for ultrasound criteria already known to be associated with thyroid cancer. The current analysis is restricted to solid, nonpalpable nodules, although the findings should apply to palpable nodules as well. The authors do not, however, provide the interobserver variability for characterization of both nodule sonographic features and diameter measurement, and they also exclude partially cystic nodules, which are quite common (up to 50% of all nonpalpable nodules); thus, applicability might be somewhat limited.
The authors also endeavor to add another sonographic feature to the list, namely an A/T≥1; however, why should the shape of a nodule matter? The ratio of surface area to volume is maximized by a spherical shape, optimizing exposure of the tumor cells to nutrients. By considering all three dimensions of a nodule (anteroposterior, transverse, and longitudinal) to calculate shape as the ratio of the longest to shortest diameter, the least spherical nodules―defined as a long-to-short axis ratio of >2.5―were found to be benign.[4] The current report only calculates the ratio of two of these three dimensions, so might not truly reflect nodule shape. Nevertheless, Cappelli et al. found that an A/T ≥1 has both high specificity (82%) and sensitivity (84%) for detection of thyroid cancer, the latter of which is significantly higher than the 33% sensitivity previously reported for this feature.[3] The use of an A/T ≥1, therefore, requires additional validation, including an analysis of interobserver variation in nodule diameter measurement, before it can be used widely to select nodules for FNAC.
Like previous reports, this study has explored sonographic criteria to identify nodules with a high cancer risk. Implicitly understood is that most nodules are not malignant. As the absolute number of detected thyroid nodules increases, the most beneficial analysis would be one that attempted to identify a subset of nodules lacking all the suspicious sonographic features for which FNAC might be omitted. Over 2 decades ago, Simeone and colleagues wrote "...the exact role of ultrasound is still to be defined ... the traditional use of ultrasound to separate cystic from solid lesions is probably outdated".[5] Although we now understand much more about ultrasound imaging of thyroid nodules, this statement remains true today. We must, therefore, begin to apply sonographic criteria to identify nodules for which FNAC is not indicated, as well as those for which it might be.
Practice Point
Sonographic features of thyroid nodules might identify lesions with a high risk of malignancy